When a person has mobility issues due to an illness, an accident, or because of old age, one of the common ailments that result from them is bed sores. When a person who has health issues acquires bed sores, it can become a serious problem, particularly for frail older adults. These can develop on skin areas that have been subjected to pressure from prolonged bed rest, wheelchair use, or cast usage.
Bed sores can also be related to the quality of care a person receives. For instance, if an immobile or bedridden person is not positioned correctly or given good skin care, bed sores can develop and worsen over time. Also, people who have circulation problems and diabetes are at higher risk when they develop bed sores.[1]
Therefore, if you have a loved one who is immobile or bedridden and have acquired bed sores, it is important that they are given the right treatment. But what are the treatment options that can be done to relieve and heal their bed sores? If you have the same question in mind, no worries, as we are here to help you. In this post, we are giving you a guide for picking the right treatments for bed sores.
Disclaimer: This article is for informational and educational purposes only and does not substitute professional medical advice. It is important to always consult a medical professional for any health issues.
What are Bed Sores?
Before we give you the tips and treatment options, let us first understand further what bed sores are. Bed sores, also known as pressure sores, develop on skin areas that are compressed from prolonged lying, sitting, or wearing of a cast. They can also be called pressure injuries, pressure ulcers, or decubitus ulcers.[1] They are very common for the elderly and those who can’t get up and move around on their own.
Bed sores develop when the supply of blood to the skin is cut off for over two to three hours. When the skin dies, the bed sore first begins as a red, painful area, which then turns purple. When it is left untreated, the skin can break open and can become infected. Bed sores can become deep and can extend into the muscle and bones. Additionally, depending on their severity, physical state, and the existence of other conditions like diabetes, bed sores typically heal slowly after they appear. This means that bed sores can take days, months, or even years to heal.
There are particular areas of the body where bed sores often occur. These include the buttocks area on the tailbone or hips, shoulder blades, heels of the feet, back of the head, and the backs and sides of the knees.[1]
The Types/Stages of Bed Sores
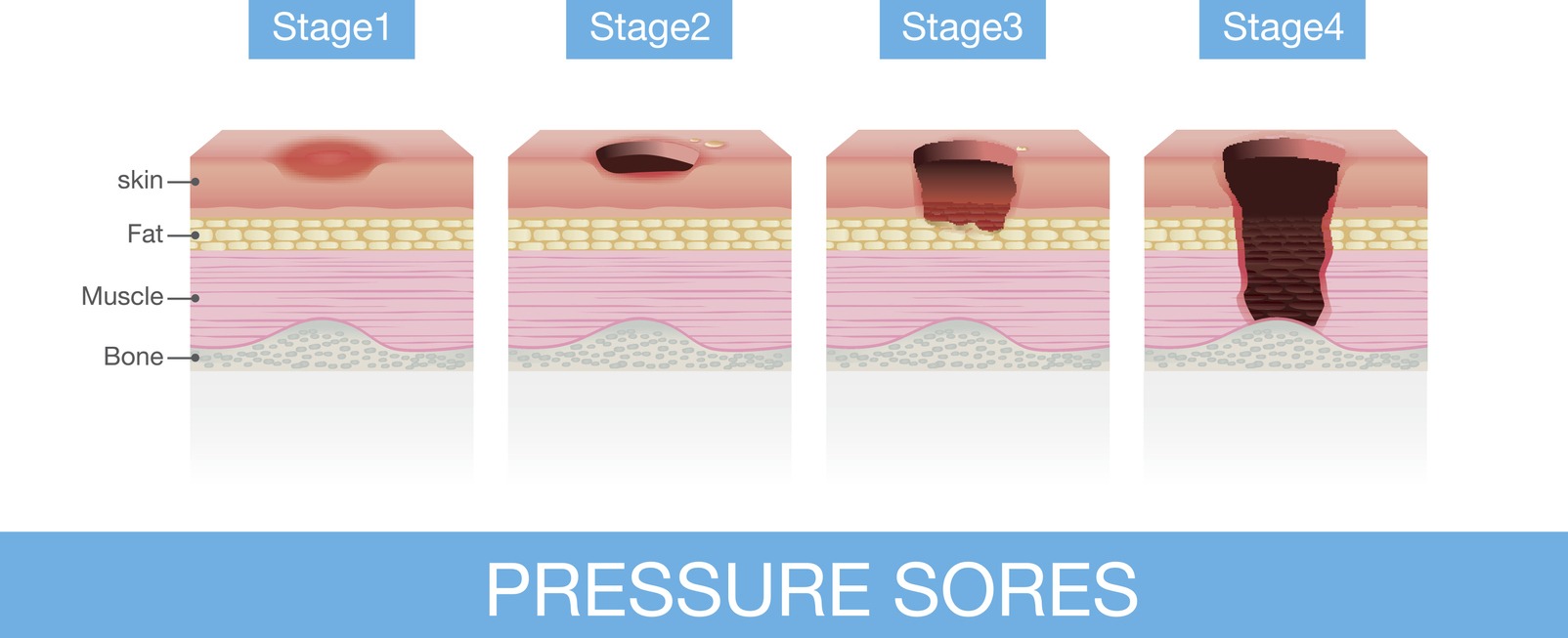
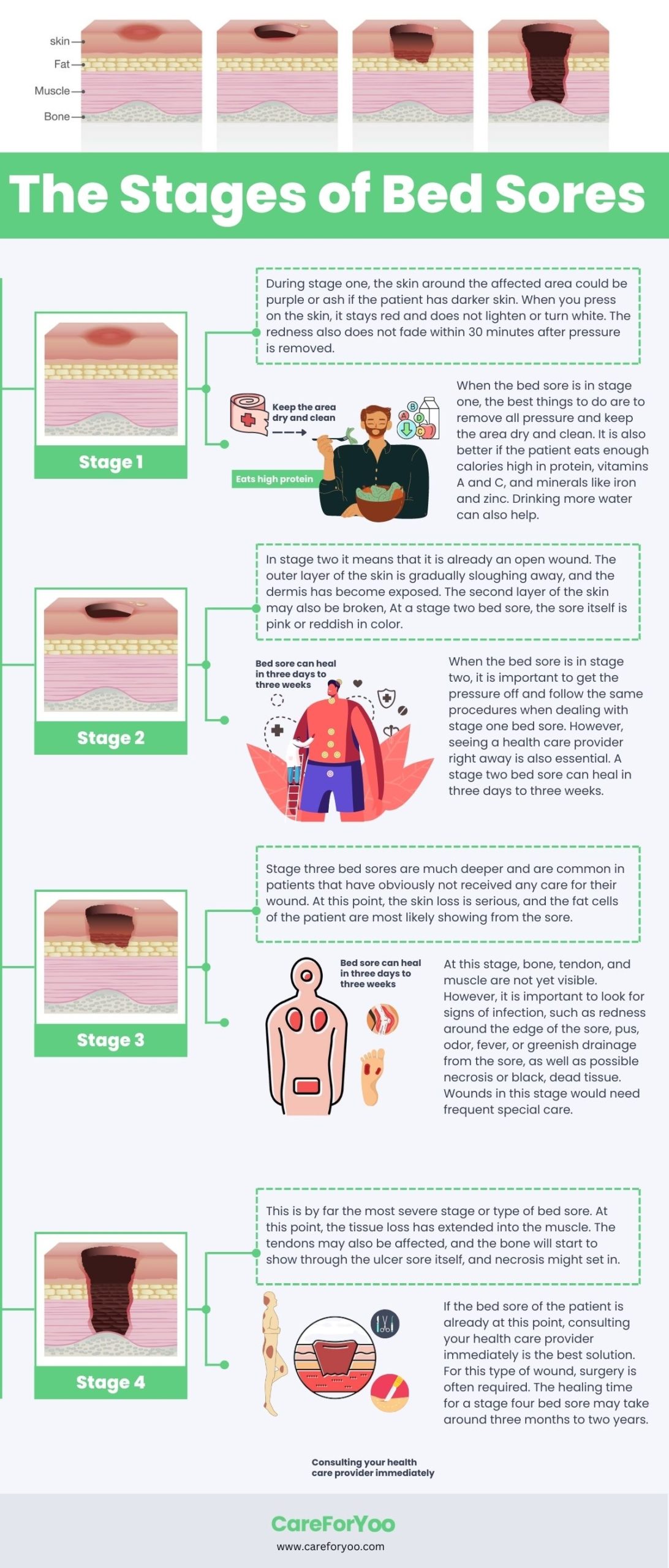
Bed sores come in four stages, and they range from minor to severe. When bed sores get more serious, it is more likely that the patient could develop a life-threatening infection. Also, the closer the bed sore gets to stages three and four, the more difficult it is to manage and treat.[2] Let us further understand the different stages of bed sores and what you can do during those stages.
- Stage 1: The stage one bed sore is one that is just beginning to form, and it is the easiest type of bed sore to treat. At this stage, the skin is not yet broken, but the sore will begin to look reddish and warm to the touch. It can also be painful as it starts to progress into stage two. During stage one, the skin around the affected area could be purple or ash if the patient has darker skin.[2]When you press on the skin, it stays red and does not lighten or turn white. The redness also does not fade within 30 minutes after pressure is removed.When the bed sore is in stage one, the best things to do are to remove all pressure and keep the area dry and clean. It is also better if the patient eats enough calories high in protein, vitamins A and C, and minerals like iron and zinc. Drinking more water can also help. A pressure sore that is just in stage one can be reversed in about three days if all pressure is taken off the affected area.[3]
- Stage 2: When the bed sore is in stage two, it means that it is already an open wound. The outer layer of the skin is gradually sloughing away, and the dermis has become exposed.[2] The second layer of the skin may also be broken, and drainage or fluid leakage may or may not be present.[3] The sore itself is shallow and treatable if addressed right away. At a stage two bed sore, the sore itself is pink or reddish in color.[2]
When the bed sore is in stage two, it is important to get the pressure off and follow the same procedures when dealing with stage one bed sore. However, seeing a health care provider right away is also essential. A stage two bed sore can heal in three days to three weeks.[3] - Stage 3: Stage three bed sores are much deeper and are common in patients that have obviously not received any care for their wound. At this point, the skin loss is serious, and the fat cells of the patient are most likely showing from the sore. If left untreated, the sore will soon deepen, and the skin tissues inside will die. Eventually, the sore will turn yellow.[2]
At this stage, bone, tendon, and muscle are not yet visible. However, it is important to look for signs of infection, such as redness around the edge of the sore, pus, odor, fever, or greenish drainage from the sore, as well as possible necrosis or black, dead tissue.[3]Wounds in this stage would need frequent special care. Therefore, you need to get the pressure off immediately and see your healthcare provider right away. It can also help if you can use a special bed or mattress for the patient. A stage three bed sore may take more than one to four months to heal.[3] - Stage 4: This is by far the most severe stage or type of bed sore. At this point, the tissue loss has extended into the muscle. The tendons may also be affected, and the bone will start to show through the ulcer sore itself, and necrosis might set in. [2] Lots of dead tissue and drainage are also present. In addition, the risk of life-threatening infection is much higher at stage four bed sore.
If the bed sore of the patient is already at this point, consulting your health care provider immediately is the best solution. For this type of wound, surgery is often required. The healing time for a stage four bed sore may take around three months to two years.[3]
What are the Ways to Treat Bed Sores?
When a patient develops bed sores, it is important to start treatment at the first sign of any symptoms. It’s because pressure ulcers are much easier to deal with when they are caught early. It is also essential to have a healthcare provider examine the affected area or areas when diagnosing suspected bed sores. There are times when surgery might be required, but it is not usually recommended as long as it has not progressed into later bed sore stages. If you are caring for a patient that suffers from bed sores, the following ways can help in treating them:
1. Frequent Repositioning
If a patient is in a chair, wheelchair, or bed for a long period, varying their position can help. This will facilitate their blood flow and reduce pressure on their boney areas, preventing the bed sore from worsening. In fact, this can be done to prevent acquiring bed sores. It is essential to be repositioned regularly so that the pressure is dispersed throughout the body.[4]
- Wheelchair Repositioning: When a patient is always in a wheelchair, shifting his weight every 15 minutes or so is important. They can go from the left to right side of their buttock or shift their position forward or backward in the chair. A wheelchair or seat cushion may also help in re-distributing pressure across their bottom. Also, using a specialty wheelchair that tilts is beneficial. They can be expensive, but they are worth it.[4]
- Bed Repositioning: If the patient is bedridden or always lying in bed due to illnesses, repositioning is also very essential to prevent bed sores from worsening. They should be adjusted between their left side, right side, and back. It is recommended to change positions every 1 to 2 hours.If the patient is not completely immobile and can move on the bed by themselves, then having a bedside rail may help them reposition themselves without assistance. Also, if possible, try to adjust the elevation of the patient’s bed. It should not be raised more than 45 degrees to prevent too much pressure on the tailbone.[4]
2. Proper Dressing and Wound Care
Another essential treatment for patients with bed sores is proper dressing and cleaning of the wound. This is because open wounds are prone to infection, and appropriate care and use of dressings will promote healing and protect the wound from bacteria. The proper care depends on the stage of the bed sore.[4]
- Stage 1: If the skin of the affected area is not broken, the best thing to do is offload pressure immediately. Then, wash the area using mild soap and water, and ask doctors for recommended moisturizers.
- Stage 2: For stage two bed sores, it is important to keep the affected area clean and dry. Using a saline rinse is also advisable to remove loose and dead tissue that surrounds the bed sore.
- Stages 3 and 4: Bed sores that are at this stage should be monitored and cared for by a health provider. They will also give specific instructions for at-home care.
3. Proper Nutrition
In addition to taking care of the wound, making good food choices also help in facilitating healing and preventing bed sores in the future. Patients suffering from bed sores should eat more foods rich in vitamins A, C, and E, such as oranges, tomatoes, strawberries, nuts, olives, broccoli, and more. Other great supplements are zinc and omega-3s for tissue repair.
In addition, maintaining a healthy weight is also essential. Most patients who are bedridden often lose body weight. This means the protection between their skin and bone will decrease. However, it is also not good to have excess weight as there will be more pressure on the body, creating a higher risk. Therefore, monitoring the weight and ensuring a healthy balance is maintained is important.[4]
4. Prevent Further Injury or Shearing
Bed sores and sensitive skin are prone to further injury, even with very minor force. During repositioning or other basic movements, patients are at increased risk of damage from friction. One of the ways that can help is by applying powder to the sheets to reduce friction. Also, avoid engaging unnecessary exposure to pressure in sore areas. Keeping the patient’s skin moisturized through hydration and using creams approved by doctors can also help.[4]
5. Incontinence Management
Limited mobility, along with incontinence, can increase the risk of infection, especially with open wounds like bed sores. To reduce bacteria exposure to the skin, diapers and incontinence pads should be used. There are also protective lotions that can be applied to shield the skin. However, in severe cases, catheters or rectal tubes may be needed, depending on what the doctor advises.[4]
6. Change Bedding and Clothing Frequently
Patients with bed sores always need to have a clean environment as they are at risk of infections. During daily checks of the skin, it is also important to change clothes and sheets to prevent bacteria from spreading. Only use sheets and clothes that are made of cotton or breathable fabric. Avoid materials that are too dense and restrict airflow.[4]
Devices/Products That Can Help Prevent or Relieve Bed Sores
When it comes to bed sores, turning or repositioning the patient is the most widely accepted treatment, and it can also be done for prevention. However, there are also other methods that exist which could strengthen the odds of an elderly resident to healing or preventing bed sores. One of these is by using devices or products, such as the following:
1. Pressure-Relieving Mattress
A lot of hospitals and long-term care facilities use special pressure-relieving mattresses for patients who are at high risk of developing pressure ulcers, such as comatose, immobile, and elderly patients and residents. These types of mattresses can alleviate pressure on the skin and increase the comfort of the patient. They also alternate pressure points periodically to prevent prolonged pressure on one part of the body.
Some pressure-relieving mattresses employ a mechanical device, such as a fixed pressure pump, to inflate and deflate the mattress’ air cells. It quietly alternates which cells receive air, reducing pressure on parts of the body throughout the day. There are also special pads that can soften the bed surface and lessen the pressure on the skin.[5]
In order to better avoid bed sores, pressure-relieving mattresses can distribute pressure away from exposed bone protrusions like the hips and the heels of the feet. If you are thinking of buying a pressure-relieving mattress, here are a few suggestions that might help you choose:
- Vive Alternating Pressure Pad: This is an example of a pressure-relieving mattress that utilizes a mechanical system to inflate and deflate its air cells. It is best for immobilized or weak patients who are unable to shift their weight frequently. It also comes with a mattress pad and an electric pump system.
- PURAP Bed Sore Mattress Pad: This one is a smaller pad that can be placed on top of an existing hospital or home mattress. It has a special technology that gives lower peak pressures than alternating pressure, gel, and foam mattress systems. It dissipates pressure and prevents skin shear, which helps heal existing bed sores.
- DMI Egg Crate Foam Mattress Topper: This mattress does not have any mechanical system. It is a simple bed topper for support, air circulation, pressure relief, and weight distribution. It is made of materials that are breathable, and the foam provides natural air circulation for a cooling effect. It can add more comfort for people who have bed sores and can be used to prevent bed sores for immobilized patients.
2. Heel-Elevating Boots
The heels of the feet are also common parts of the body for bed sores, especially for the elderly. It’s because the weight of the feet pushes through the heels on bed rest, which leads to excessive pressure that damages or destroys the skin tissue on the heels. To prevent the bed sores on the heels from worsening, using heel-elevating boots can help.[5]
Heel-elevating boots are used to suspend feet in midair, redistributing pressure to the calf to prevent the further development of pressure ulcers. It is a piece of equipment that supports and cushions the foot, ankle, and lower leg to lessen the possibility of skin friction and pressure points. Below are some product examples that might help you choose:
- Heel Keeper 2: These heel-elevating boots are lightweight and can help prevent and treat pressure ulcers on the feet or heels. It has a calf-cradling foam cushion that elevates the heel above the resting surface. Also, the heel and foot are uncovered, which can easily allow the patient to walk or stand, if they can, without removing the device.
- McKesson Heel Protector Boot: This heel protector boot has a hook-and-loop closure that provides various ways to secure the boot. It has three holes on each side to accommodate deep vein thrombosis pressure devices, including cuffs and massagers. It surrounds the foot with a soft cotton material to avoid friction on the skin and provide air circulation to help heal existing sores.
- NYOrtho Heel Protector Cushion: These heel-elevating boots have an extended and cushioned design that elevates the heel over an air cavity for zero pressure. They also provide air circulation to help in the healing of existing ulcers. They are made of soft velvet fabric to protect the skin from tears and to reduce friction and shear.
3. Special Cushions
Sitting or lying on softer surfaces is sometimes all it takes to treat and prevent bed sores. Therefore, placing special cushions or pillows beneath the pressure points of the patient can relieve pressure and enable adequate blood supply to those parts.[5] There are specifically designed cushions available in the market that are made to help treat and prevent bed sores. They can fit in wheelchairs, seats, or on beds. Some of them are made with gel or memory foam to promote blood flow. Below are some options that may help you choose the right special cushion:
- TURNSOLE Wheelchair Cushion for Pressure Sores: If the patient spends long periods sitting in a wheelchair, this product can help relieve pressure sores or prevent them from developing or worsening. It is a wheelchair cushion that is made of breathable, comfortable, and durable materials. It is designed to disperse body pressure. It also comes with a special pump to inflate the cushion.
- DMI Egg Crate Sculpted Foam Chair Cushion: If a patient spends a lot of time sitting on a chair or on the bed, this cushion seat may help alleviate the symptoms of bed sores. It is made of medical-grade egg crate foam that can help reduce or heal pressure sores by taking the weight off sensitive areas and improving air circulation. It can be used on wheelchairs, car chairs, kitchen chairs, and office chairs.
- FANWER Bed Wedge Pillow: This is a special pillow that is great for patients who are bedridden. It is a side wedge pillow made of high-grade and breathable fabric. It can help patients turn over, change their position, assist with passive leg lifting, and improve leg blood circulation. It can be used to reposition patients with bed sores easily in bed.
4. Skincare Products
While pressure is the main cause of bed sores, there are also some skin conditions that contribute to the development of painful bed sores. These include skin that is too dry, moist, dirty, and brittle, as they are more prone to sores and lesions. With this, it is also essential to use skincare products that can give protection to the skin, as well as treat and prevent bed sores.[5]
One example of a skincare product for patients suffering from bed sores is a cleansing body lotion. This is essential, especially for those suffering from incontinence and bed sores, as it can prevent moist and unsanitary skin. There are no-rinse cleansing solutions available in the market today that can keep an individual clean and protected from incontinence, which in turn prevents the infection of bed sores.
In addition to that, antimicrobial cleansers can also be used to avoid infections. There are special antimicrobial skincare products available that help eliminates bacteria and fight infections near bed sores. Skin protectants can also be used to provide a barrier for irritated or sensitive skin. Applying them to the affected area can protect the bed sores against excess moisture, water loss, pain, inflammation, and bacteria.[5] There are many different skincare products available in that market that can be beneficial for patients with bed sores. Below are some suggestions to help you choose:
- SkinSmart Antimicrobial Perineal Cleanser: If the patient with bed sores also suffers from incontinence, this skin cleanser might help. It is a rinse-free solution made for incontinence to avoid infections, particularly if bed sores are present. It is easy to use as it utilizes an easy touch-free spray. It can help in keeping the patient’s skin clean at all times.
- Terrasil Bed Sore Treatment Cream: This is a soothing ointment made of natural ingredients. It promotes fast healing of bed sores and pressure sores. In addition, it is also a skin protectant that can act as a barrier against infection, which is the main cause of delayed healing in wounds.
- Hess Moisturizer for Bed Sore Prone Skin: If the bed sore is just starting or just at stage one, using a moisturizer like this can help prevent it from developing further. This moisturizer is made with all-natural ingredients that are safe for the skin. It keeps the skin hydrated and prevents it from drying and cracking, which can lead to worsened bed sores.
Conclusion
Bed sores are indeed among the painful and potentially very serious medical conditions, especially for the elderly who are immobilized or bedridden. While they are treatable, mishandling them can lead to medical complications. Therefore, to prevent further health issues from developing due to bed sores, it is important to address and treat them immediately.
Relieving pressure on the affected area is the most important step in treating bed sores, along with keeping it dry and clean at all times. There are also lots of products and devices that can help the patient strengthen the skin’s protective barriers to prevent bed sores from developing further, such as creams and lotions. These products, combined with pressure-relieving cushions, mattresses, and other devices, can be enough to help someone in treating and avoiding bed sores. We hope this post helped you learn more about picking the right treatments for bed sores.
References
[1] Johns Hopkins Medicine, E. (2021, August 8). Bedsores. Johns Hopkins Medicine. Retrieved September 20, 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/bedsores
[2] Koonz Mckenney Johnson & Depaolis, E. (2022, February 23). The various types of bedsores and how they occur. Koonz McKenney Johnson & DePaolis LLP. Retrieved September 20, 2022, from https://koonz.com/various-types-bedsores-occur/
[3] MSKTC, E. (n.d.). Recognizing and treating pressure sores. Recognizing and Treating Pressure Sores | Model Systems Knowledge Translation Center (MSKTC). Retrieved September 20, 2022, from https://msktc.org/sci/factsheets/skincare/Recognizing-and-Treating-Pressure-Sores
[4] Jessica, H. (2017, January 26). Bed sores treatment [ultimate guide]. Vive Health. Retrieved September 20, 2022, from https://www.vivehealth.com/blogs/resources/bed-sore-treatment
[5] Nursing Home Law Center, E. (2022). What devices or products can be used to prevent or relieve bed sores? Nursing Home Law Center. Retrieved September 20, 2022, from https://www.nursinghomelawcenter.org/what-devices-or-products-can-be-used-to-prevent-or-relieve-bed-s.html